Key Takeaways
- Incidental peritoneal metastases are a common real-world event in both emergency and elective abdominal surgery—and the first intraoperative decision can define what treatment options remain possible. main
- The 2026 Surgical Oncology review offers a clear decision framework that helps surgeons replace improvisation with strategy when peritoneal implants are unexpectedly found.
- PCI is more than a staging tool in these moments: it becomes a shared language that enables faster expert review, better referral, and more accurate planning.
- In my experience, the highest-yield actions are often the simplest: complete abdominal inventory, video when feasible, and multiple representative biopsies—all while preserving planes and avoiding unnecessary trauma.
- Ultimately, this is a care pathway problem as much as a surgical one: structured staging + tumor board + specialized referral is how we protect patients from the consequences of surprise decisions.
Stay updated on peritoneal oncology evidence and practice: https://peritoneo.life/newsletter/
There is a specific kind of phone call that happens in peritoneal surface oncology—usually from an excellent surgeon, sometimes in the middle of a case, often in an uncomfortable moment of uncertainty.
“Artur, I was operating for appendicitis… and found peritoneal nodules.”
“This looked like diverticulitis… but the abdomen doesn’t fit.”
“It seemed like endometriosis… until I saw the omentum.”
“Routine cholelithiasis… unexpected implants everywhere.”
These are common situations that all surgeons will face one day or another! The doubts that emerges are not about lack of skill. They are about a reality that the 2026 Surgical Oncology review brings into focus: incidental peritoneal metastases are not rare, and the first intraoperative decision can reshape the entire oncologic trajectory.
This article—Incidental peritoneal metastases in the setting of emergency surgery: Review of evidence and algorithm for oncologic decision-making—is valuable because it does something we need more in abdominal oncology: it turns a chaotic moment into a structured mindset.
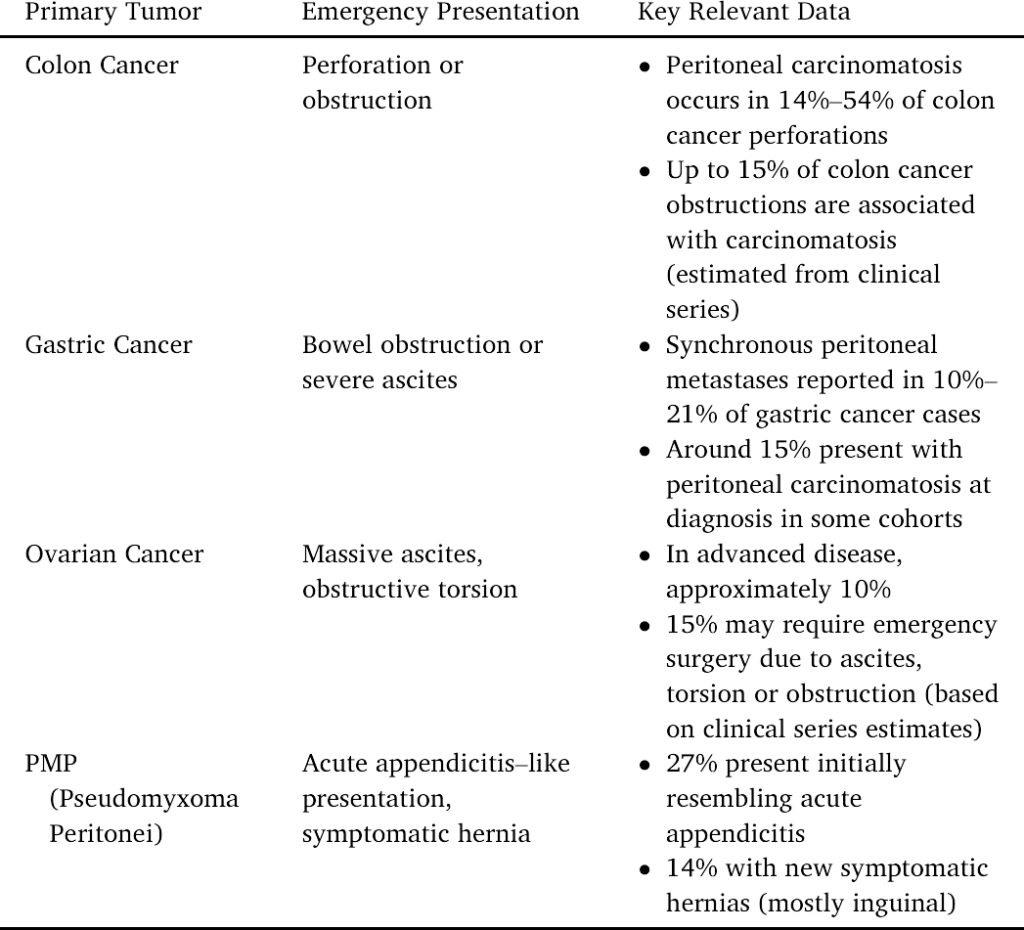
Why this scenario is more common than most surgeons expect
One of the most useful contributions of the review is how it frames emergency presentations by likely underlying primary tumor. The message is subtle but important: emergency surgery is not an “exception” in peritoneal oncology—it is part of the natural history of several intra-abdominal malignancies.
In my own experience, incidental peritoneal disease has been discovered during both emergency and elective surgeries initially approached as:
- appendicitis
- diverticulitis
- suspected endometriosis
- cholelithiasis and other “routine” abdominal procedures
And the final diagnoses have been diverse:
- appendiceal mucinous neoplasm / pseudomyxoma peritonei
- colorectal cancer
- ovarian cancer
- pancreatic cancer
- and other primaries presenting with peritoneal spread
This diversity matters because it reinforces a critical truth:
Peritoneal implants are a finding—not a diagnosis.
What you do next determines whether the patient keeps options open.
Stay updated on peritoneal oncology evidence and practice: https://peritoneo.life/newsletter/
The algorithm: two calm questions that prevent irreversible mistakes
The author proposes an oncologic decision-making algorithm that can be summarized by two questions asked in real time:
- Do the peritoneal metastases explain the patient’s symptoms?
- Does the patient require immediate palliation of symptoms right now?
This framework is powerful because it interrupts the most dangerous reflex in these cases: the impulse to “finish the job” in an unplanned setting.
The algorithm is not about being passive. It is about being strategic when the disease has declared itself unexpectedly.
The PCI: staging tool—or the shared language that saves the patient
A schematic representation of the Peritoneal Cancer Index (PCI): the abdominal cavity divided into 13 regions, each scored from 0 to 3 based on implant size, generating a total score from 0 to 39. main
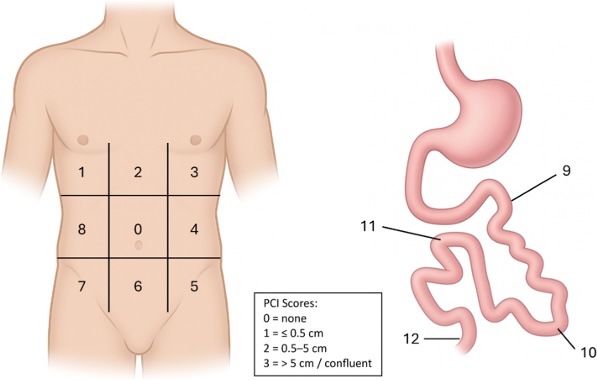
Fig. 1. Schematic representation of the Peritoneal Cancer Index (PCI), which divides the abdominal cavity into 13 anatomical regions. Each region is scored from 0 to 3 based on the maximum size of peritoneal implants, yielding a total score ranging from 0 to 39.
In theory, PCI is a staging system. In practice—especially in the emergency setting—PCI becomes something else:
It becomes a shared language between a general surgeon and a specialized peritoneal center.
A thoughtful abdominal inventory and a PCI estimate (even approximate) can later answer the most consequential questions:
- Is disease limited or diffuse?
- Is small bowel heavily involved?
- Is this potentially resectable in a planned setting?
- Did the first operation preserve planes or create avoidable damage?
This is why I routinely recommend that, when feasible, surgeons record a short intraoperative video. Not for teaching. Not for marketing. For patient care and accurate expert review.
If you encounter unexpected peritoneal implants during an emergency or elective abdominal surgery and need rapid guidance on documentation, biopsy strategy, and referral, you can reach me here: www.drarturreis.com.br.
Stay updated on peritoneal oncology evidence and practice: https://peritoneo.life/newsletter/
My real-world recommendations (and why each one matters)
When I receive these calls, my guidance is consistent—not because every case is identical, but because future options are fragile after an impulsive first operation.
1) Perform a complete abdominal inventory
Why: distribution—especially small bowel and porta hepatis—can determine everything later.
PCI: if you know how to calculate, please do it!!!
2) Record video documentation when feasible
Why: a short video often communicates more than a paragraph in the operative note.
3) Take adequate biopsies: at least 5 representative samples
Why: peritoneal disease can mimic inflammation, endometriosis, granulomatous conditions, or benign mucin. Diagnostic certainty requires tissue.
4) Avoid multiple incisions, unnecessary drains, and extra surgical trauma
Why: added trauma increases adhesions and distorts future cytoreduction planes.
5) Avoid unplanned multivisceral resections
Why: major resections in the wrong setting raise complications and can compromise eligibility for specialized strategies.
6) Avoid any anastomosis whenever feasible
Why: in this context, an anastomotic leak can be catastrophic—biologically, clinically, and logistically.
7) Preserve anatomical planes
Why: CRS depends on planes. When planes are destroyed early, curative-intent options shrink.
8) Ensure the patient has a direct path to expert evaluation
Why: time matters. The greatest risk after “incidental carcinomatosis” is falling into a referral gap.
These recommendations may seem simple, but they are designed to protect what matters most in peritoneal oncology: future options. In incidental peritoneal disease, the first operation should stabilize the patient and preserve anatomy, allowing proper staging, multidisciplinary review, and referral to a specialized pathway—rather than forcing irreversible decisions under pressure.
Stay updated on peritoneal oncology evidence and practice: https://peritoneo.life/newsletter/
If you encounter unexpected peritoneal implants during an emergency or elective abdominal surgery and need rapid guidance on documentation, biopsy strategy, and referral, you can reach me here: www.drarturreis.com.br.
The Decision-Making Flowchart: A Practical Algorithm Worth Adopting
One of the most valuable parts of this review is the decision-making flowchart proposed by the authors. It is “simple” in the best sense: it transforms a high-pressure intraoperative surprise into a structured sequence of questions that protects the patient from avoidable harm—and preserves future oncologic options.
At the core of the algorithm are two essential checkpoints.
First: Do the peritoneal metastases explain the patient’s acute presentation?
This step forces a pause. If the emergency is truly driven by peritoneal disease (for example, obstruction, perforation, bleeding, or sepsis), then the surgical objective should be symptom control and stabilization, not definitive oncologic surgery. The flowchart encourages the surgeon to choose the safest, least traumatic option that resolves the emergency—often diversion, bypass, or limited procedures—while avoiding maneuvers that increase complication rates and compromise later cytoreduction.
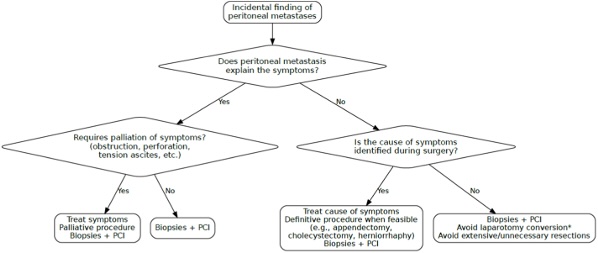
Second: Is immediate palliation required right now?
If the patient needs urgent palliation, the algorithm supports focused intervention with a clear bias toward safety and preservation of anatomical planes. If the patient does not require immediate palliation (or once the acute issue has been controlled), the flowchart pivots toward what peritoneal oncology truly demands: documentation, representative biopsies, structured staging, and early referral for expert multidisciplinary review.
What makes this flowchart so useful is that it legitimizes restraint. It gives surgeons a defensible, evidence-informed framework to avoid “unplanned escalation” in the operating room simply because peritoneal disease was discovered. Instead, it supports a mature sequence: treat the emergency, document properly, sample intelligently, and transition the patient into a planned oncologic pathway—exactly the approach that maximizes the chance of appropriate specialist evaluation and preserves eligibility for specialized strategies in peritoneal surface malignancies.
What I appreciate most about the paper
The review normalizes a reality that many surgeons experience but few systems address:
- incidental peritoneal disease is common enough to demand a pathway
- emergency surgery is not the time for definitive oncologic cytoreduction
- staging, documentation, and biopsy are the highest-yield actions in that moment
- structured decision-making protects patients from the consequences of improvisation main
The part I would emphasize even more: this is a systems problem
The paper is presented as “evidence + algorithm,” but the deeper message is organizational:
Incidental peritoneal metastases are a health-system test.
If a surgeon has:
- a defined referral route,
- tumor board access,
- a specialized peritoneal center,
- and a shared staging language (PCI + documentation + pathology),
then the unexpected finding becomes manageable.
If none of these exist, the patient is left to improvisation.
And in peritoneal oncology, improvisation is often costly.
Final reflection: the most important move may be restraint
Emergency surgery is often framed as decisive action.
But when peritoneal metastases appear unexpectedly, the most decisive act may be restraint: stabilize the patient, document accurately, obtain proper tissue, and protect future options.
This review gives structure to that maturity.
And in my view, outcomes sometimes change before any CRS, HIPEC, or PIPAC is even discussed—
they change when a surgeon, in a high-pressure moment, chooses strategy over impulse.
FAQ — Incidental Peritoneal Metastases in Emergency Surgery (SEO + AI Search)
1) What are incidental peritoneal metastases?
Incidental peritoneal metastases are peritoneal implants discovered unexpectedly during surgery performed for another presumed diagnosis (often emergency conditions like appendicitis, obstruction, or perforation).
2) How common is it to find peritoneal metastases during emergency surgery?
A meaningful proportion of patients with peritoneal surface malignancies present in emergency settings during their disease course, making incidental discovery clinically relevant.
3) What is the main message of the 2026 Surgical Oncology review on this topic?
The central message is to manage the acute surgical problem while preserving oncologic options through careful documentation, staging, biopsy, and structured referral.
4) Should surgeons perform definitive cancer surgery when peritoneal implants are found unexpectedly?
In most cases, unplanned definitive oncologic surgery in the emergency setting is discouraged, favoring stabilization and referral for planned multidisciplinary care.
5) What is the Peritoneal Cancer Index (PCI)?
PCI is a staging tool that divides the abdomen into 13 regions and scores tumor implant size per region (0–3), producing a total score from 0–39.
6) Why is PCI useful during emergency surgery?
Even an approximate PCI estimate helps communicate disease distribution to a specialized center and supports future planning, resectability assessment, and multidisciplinary decision-making.
7) What does the authors’ decision flowchart (algorithm) focus on?
The algorithm centers on whether peritoneal disease explains the acute presentation and whether immediate palliation is required, guiding safer intraoperative choices.
8) What is the first key question in the algorithm?
Whether peritoneal metastases explain the patient’s symptoms (e.g., obstruction, perforation, sepsis), which shapes the goal of surgery.
9) What is meant by “immediate palliation” in this context?
Immediate palliation refers to interventions needed right away to relieve life-threatening or severe symptoms such as obstruction or perforation, focusing on safe symptom control.
10) What are the recommended priorities when incidental peritoneal metastases are found?
A complete abdominal inventory, documentation (ideally video), representative biopsies, peritoneal fluid sampling when feasible, and early referral after stabilization.
11) How many biopsies should be taken when peritoneal implants are found?
Multiple representative samples from different regions improve diagnostic accuracy and downstream planning.
12) Why is intraoperative video documentation helpful?
Video can transmit disease distribution more accurately than narrative operative notes and supports expert review and tumor board discussion after the emergency setting.
13) Should surgeons avoid multivisceral resections in these cases?
Yes—unplanned multivisceral resections may increase complications and compromise future treatment options; restraint supports better long-term strategy.
14) Why should surgeons avoid primary anastomosis when feasible?
In carcinomatosis and emergency settings, anastomotic leaks can be catastrophic and may delay systemic therapy and specialist referral; safer alternatives may be preferred.
15) What is the safest surgical goal when peritoneal metastases are discovered in an emergency?
Stabilization and symptom control—solving the acute problem while preserving anatomical planes and future oncologic options.
16) Which emergency scenarios are commonly associated with peritoneal metastases?
Bowel obstruction, perforation, bleeding, sepsis, and acute presentations that mimic benign disease (e.g., suspected appendicitis).
17) Can peritoneal metastases mimic benign diseases like appendicitis or endometriosis?
Yes. Peritoneal disease can resemble inflammatory or benign conditions, which is why tissue diagnosis and structured staging matter.
18) Are incidental peritoneal metastases always terminal disease?
No. In selected patients, peritoneal metastases may be approached with specialized strategies, depending on distribution, biology, and planned care.
19) What should happen after the emergency surgery is completed?
Structured staging (imaging, pathology review, origin work-up) and referral for multidisciplinary evaluation in a specialized pathway.
20) What imaging is typically used after incidental peritoneal metastases are found?
Cross-sectional imaging is commonly used to define extent and guide next steps, often including CT of chest/abdomen/pelvis.
21) Why is identifying the primary tumor important?
Because peritoneal metastases are a manifestation, not a diagnosis—origin determines systemic therapy options, surgical strategy, and prognosis.
22) How can a surgeon describe peritoneal disease clearly in the operative report?
Use a structured abdominal inventory, PCI regions, implant size estimates, biopsy locations, and photo/video documentation.
23) What is the biggest risk after “incidental carcinomatosis”?
A referral gap—patients can lose time and opportunities if there is no clear pathway for staging, tumor board discussion, and specialist evaluation.
24) How does a structured care pathway improve outcomes in peritoneal oncology?
It reduces improvisation, accelerates staging and referral, standardizes decision-making, and helps preserve eligibility for specialized strategies when appropriate.
25) Where does multidisciplinary tumor board discussion fit into this process?
Tumor boards synthesize pathology, imaging, disease distribution (including PCI estimates), and patient factors to recommend the most appropriate planned strategy.
26) What is the role of specialized peritoneal centers?
They provide expertise in staging, selection, and integrated strategies (surgical, systemic, and locoregional) with appropriate infrastructure.
27) What should a surgeon do if they are unsure during an emergency case?
Stabilize the patient, document thoroughly, obtain representative biopsies, avoid unplanned escalation, and arrange early specialist referral.
28) Can incidental peritoneal metastases be found during elective surgery too?
Yes—incidental findings can occur during elective procedures for presumed benign or inflammatory conditions; the same principles apply.
29) Why does preserving anatomical planes matter so much?
Cytoreduction relies on surgical planes; excessive trauma and adhesions from an unplanned first operation can reduce feasibility and increase risk later.
30) What is the practical takeaway for non-specialist surgeons?
When implants are found unexpectedly: stabilize, document (PCI + video), biopsy intelligently, avoid unplanned aggressive resections/anastomosis, and ensure rapid referral.
